We are living through one of the biggest pandemics the world has ever known, yet many people do not even realize it. You or someone close to you may already be caught in its grip. I am not talking about a virus. I am talking about a mental health crisis that continues to grow quietly all around us.
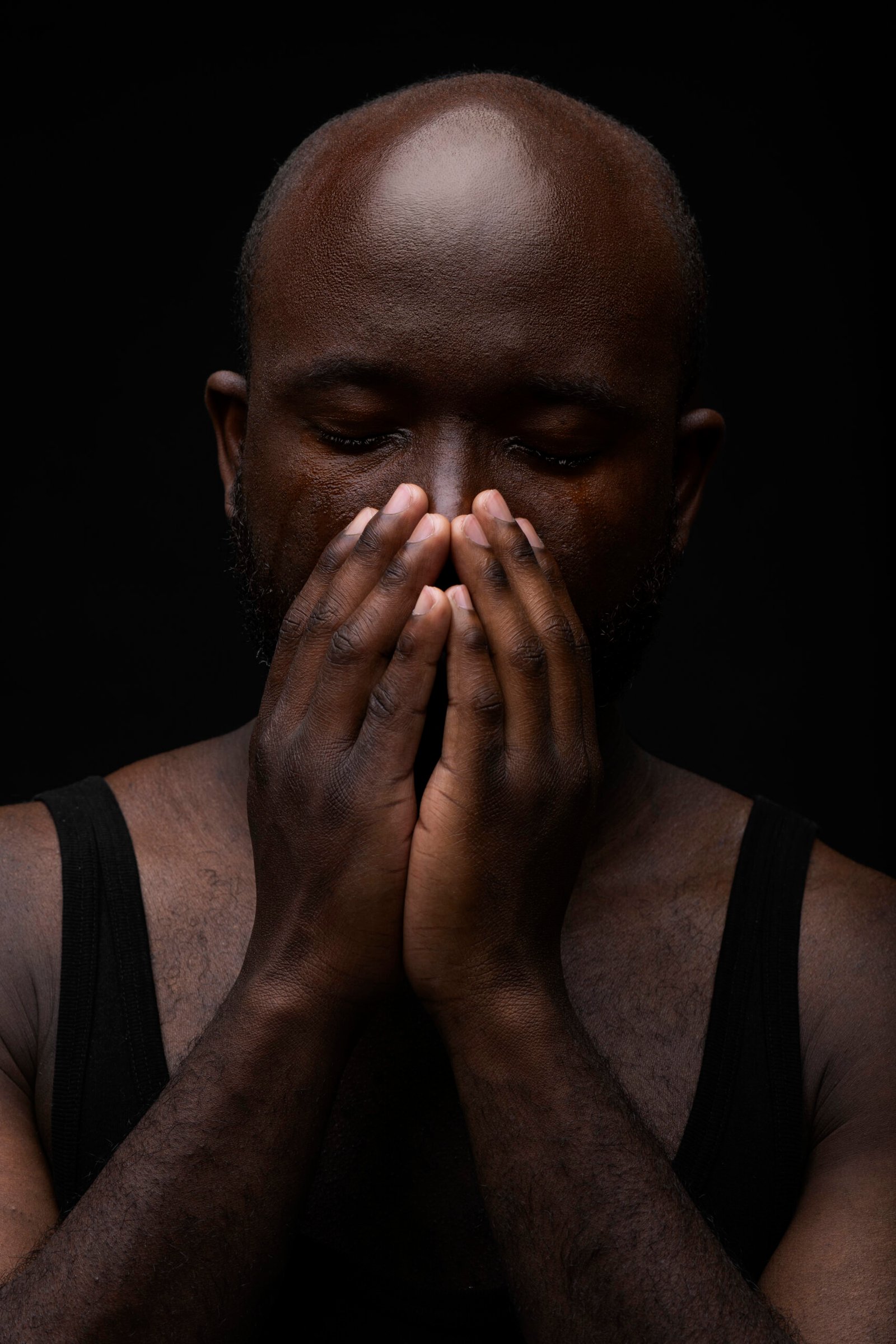
Half of us who struggle with mental health challenges will never seek help. Some of us stay silent because of stigma. Others simply do not recognize what is happening inside us until the pain becomes too heavy to carry. This silence keeps too many people suffering in isolation, believing that struggling means they are weak. That is not true. Struggling means you are human.
Understanding the Crisis
It may surprise you to hear that the number of serious mental illnesses such as schizophrenia or major depression has not drastically increased. What has increased is our willingness to do something about them. More people are reaching out, asking for help, and acknowledging what they feel. That is a powerful step forward.
For a long time, many were told to just tough it out, to keep moving, to hide their emotions. Today, more people are realizing that ignoring mental health only deepens the wound. When you recognize that something is not right and you take steps to address it, you are already moving toward healing.
When we finally encourage people to come forward, we see how great the need truly is. The demand for mental health support is higher than ever. That is not a sign that the world is falling apart. It is a sign that people are finally ready to stop suffering in silence.
Getting help does not mean you are broken. It means you are taking responsibility for your well-being. Whether you choose therapy, support groups, mindfulness practices, or conversations with trusted people, every step counts. What matters most is that you do not face this alone.
Building a Healthier Mindset
We need to move away from the idea that asking for help shows weakness. Instead, let us recognize that it takes courage to admit when we are not okay. Talking about mental health openly allows others to see that they are not alone. It helps build a culture of compassion where healing becomes possible.
Start with awareness. Notice how you are feeling. Pay attention to changes in your sleep, mood, or energy. Reach out to someone you trust. And if you are supporting someone who is struggling, remember that listening is one of the most powerful things you can offer.
We are in serious trouble when it comes to mental health across the world, but we are also in a time of incredible opportunity. The more we talk about it, the more we break down barriers that keep people silent. Each honest conversation helps to replace shame with understanding and hopelessness with hope.
Let us stop pretending everything is fine when it is not. Let us stop judging ourselves and others for needing help. Healing begins when we choose to face our pain with honesty and care.
You are not alone in this. Help is available, healing is possible, and together we can create a world where taking care of our mental health is as normal as taking care of our bodies.
Understanding Depression and When to Seek Help
Let us take a moment to talk honestly about mental health. Many people are struggling right now, and it is important to remember that there is no single path to recovery. What matters most is that you take the first step and start the conversation.
When you begin to talk about what is happening, the next step is to figure out what kind of support you need. Sometimes it may be a short-term issue that can improve with counseling or changes in your daily routine. Other times, it may be something more serious, such as a major depression, that requires a wider range of treatments like therapy, medication, or both.
It can also be the case that more than one issue is happening at the same time. For example, depression and anxiety often appear together. In those moments, the goal is to identify what needs attention first and how treatments can be sequenced to help you recover safely and steadily.
The most important thing is that you are willing to come forward and talk. That single decision can open doors to understanding and healing.
What Depression Really Is
Among all mental health concerns, depression is one of the most common. We hear about it often, but the word itself can be misunderstood. Feeling sad or low from time to time is part of being human. Everyone experiences ups and downs in life. Those difficult days do not automatically mean you are depressed.
Depression becomes a concern when those feelings of emptiness, exhaustion, or loss of pleasure last a long time, feel severe, and begin to affect how you function day to day. You may find that things you once enjoyed no longer bring satisfaction. You may struggle to focus, feel constantly fatigued, or sense that something inside you is simply “not right.”
Depression and anxiety often travel together. You might notice a constant undercurrent of worry, restlessness, or tension alongside feelings of sadness or hopelessness. These two conditions can overlap, which is why professional assessment can help clarify what is really happening and guide treatment effectively.
You Do Not Have to Look Depressed to Be Depressed
One of the biggest misconceptions about depression is that it always looks obvious. People may say, “You can’t be depressed, you’re always smiling.” The truth is that many people who are depressed appear outwardly fine. They may continue to work, care for their families, and even joke with friends while quietly suffering inside.
This silent struggle often happens because of stigma or because people feel they must hold everything together for others. Some may not even realize they are depressed because they have never experienced it before or come from a background where mental health is not openly discussed.
When depression becomes severe, those around you may begin to notice changes in your mood, energy, or ability to function. But before it reaches that point, the signs can be subtle, which is why self-awareness is so important.
Recognizing When to Get Help
Ask yourself a few honest questions.
-
Are my low feelings unusually intense or lasting much longer than usual?
-
Have I lost interest in things that normally bring me joy?
-
Am I having trouble concentrating or keeping up with responsibilities?
-
Have loved ones noticed that I seem different?
If the answer to several of these is yes, it may be time to talk to someone you trust. Ask them what they notice about you. Sometimes others see the changes before you do. If they share concerns, consider reaching out to a healthcare professional such as a family doctor, nurse practitioner, or mental health counselor.
Seeking help is not a sign of weakness. It is a sign of awareness and strength.
What Treatment Looks Like
If depression is identified, treatment options will vary depending on your situation. For some people, talk therapy especially cognitive behavioral therapy can be very effective. It helps you recognize patterns of thought that may be keeping you stuck and gives you tools to respond in healthier ways.
For others, medication may be helpful, particularly when symptoms are severe or persistent. It is important to remember that antidepressants do not treat ordinary sadness. They are designed for clinical depression, which affects brain chemistry and functioning in a deeper way.
Both therapy and medication can be effective, and often the combination works best. The good news is that most people who seek help recover fully and return to their normal lives.
Understanding Anxiety and Effective Therapy
Before moving on to anxiety, it is important to understand that not all therapies are equally effective. Unfortunately, not every therapist or counselor follows evidence-based models that have been proven to work. This is why it is valuable to learn what effective treatment should look like for your specific condition.
If you are receiving therapy, ask questions such as:
-
What type of therapy are we using?
-
Is it supported by research for the condition I have?
-
How will we know if it is working?
As a client, you have every right to ask these questions. Effective therapies for depression, anxiety, and other mental health conditions are well established. In Ontario, Health Quality Ontario has developed clear quality standards that describe what good care should look like. These standards also outline questions you can ask your care provider. If you find that what you are receiving does not align with those standards, it is appropriate to discuss this directly with your provider and ask how your treatment plan can be improved. If necessary, you can seek another opinion or a different therapist who uses evidence-based approaches.
Remember that you are an active participant in your care. Your voice matters in shaping your path toward recovery.
Moving From Depression to Anxiety
Many people assume that depression and anxiety are the same, but they are not. Depression often involves persistent sadness, loss of motivation, or loss of pleasure in life. Anxiety, on the other hand, is usually a state of excessive worry or fear about what might happen in the future.
Even though they are distinct, they often appear together. Someone who is depressed may develop anxiety, and someone with an anxiety disorder may become depressed over time. Substance use can also enter this cycle, as some people try to manage their symptoms with alcohol or drugs. The problem is that this often makes things worse and can lead to dependency or further emotional distress.
When anxiety becomes the main source of distress, it deserves focused attention and treatment on its own. The symptoms may include restlessness, muscle tension, trouble sleeping, difficulty concentrating, and an ongoing sense of dread or unease.
Understanding Panic Attacks
One specific form of anxiety is the panic attack. A panic attack is a sudden episode of intense fear that is accompanied by strong physical sensations. These may include:
-
A racing or pounding heart
-
Shortness of breath
-
Sweating or trembling
-
Dizziness or lightheadedness
-
Numbness or tingling in the hands or face
-
Feeling detached or unreal
-
A sense of impending doom or fear of dying
Panic attacks usually come on suddenly and may last around 10 to 20 minutes, although they can feel much longer in the moment. They can be frightening, especially if it is your first time experiencing one. Some people mistake panic attacks for heart problems or other medical emergencies because the symptoms can be so intense.
If you experience these symptoms, it is important to seek professional evaluation. Panic attacks are treatable. Cognitive behavioral therapy, relaxation techniques, breathing exercises, and in some cases medication can help reduce both the frequency and severity of attacks.
Taking Control of Your Mental Health
Whether you are dealing with depression, anxiety, or both, the first step is awareness. Learn about the condition, ask informed questions, and take an active role in your care. The more you understand about how mental health works, the better prepared you are to manage it.
You deserve effective, compassionate, and evidence-based care. If what you are receiving does not feel right, speak up, ask questions, and advocate for yourself. Healing begins when you become an informed and empowered partner in your own mental health journey.
The Importance of Investing in Mental Health and Finding Hope
Many people experience a panic attack at least once in their lives. For most, it is an isolated event that does not turn into a serious or disabling condition. However, when panic attacks become frequent, and when people begin to fear having another one, the problem can grow. If that fear extends to being outside or in public places, it can lead to agoraphobia, which is when the person avoids certain situations because of the fear of experiencing panic in front of others. At this point, it becomes a clinical condition that requires proper care and attention.
Why Mental Health Deserves Equal Attention
We often invest time and money into our physical health. We monitor our diet, make time for exercise, and go for medical checkups. Yet, we tend to neglect our mental health, even though it has a direct effect on how we think, feel, and function every day. Governments and health systems have also historically underfunded mental health services. For many years, mental health care was limited to institutional settings, while the majority of public health spending went toward physical illnesses.
That approach has been a mistake. When we care for our mental health, we improve our overall health. People who receive timely and effective mental health care often experience better physical outcomes as well. Studies from around the world have shown that health systems that integrate mental health with primary care produce better results for patients and communities.
The Economic Impact of Mental Health
The burden of mental illness and substance use is greater than many realize. The Mental Health Commission of Canada reports that in Ontario, the disease burden from mental illness and substance use is about one and a half times higher than all cancers combined and more than seven times higher than infectious diseases.
These numbers are not just about the cost of treatment. Mental health conditions often have long-term effects on a person’s ability to work and maintain daily responsibilities. Depression, anxiety, and other mental health issues are now leading causes of workplace absence. When people cannot access help, the cost is not only personal but also economic. Lost productivity, unemployment, and long-term disability all stem from untreated mental health problems.
Investing in mental health is therefore not only a moral responsibility but also a sound economic strategy. When people are mentally healthy, they are more productive, engaged, and able to contribute fully to their families and communities.
Finding Hope When Help Feels Out of Reach
It is understandable to feel frustrated. Many people face long waiting lists for counseling or psychiatric care. For some, the cost of private therapy is simply too high. Others feel lost in the system, unsure where to turn.
If you are in this situation, remember that you are not alone and that help can take many forms. Start by talking to your primary care provider about available supports in your area. Community organizations, peer support networks, and virtual counseling options may be more accessible than you think. Even small steps, such as speaking with someone you trust, practicing self-care, and learning about mental health through reliable sources, can make a meaningful difference.
And most importantly, hold on to hope. Recovery is possible. Most people who seek help for depression, anxiety, or panic-related issues improve significantly. Mental health challenges do not define who you are. With patience, support, and the right care, you can regain stability and rebuild your sense of purpose and connection.
Hope is not a vague promise. It is the foundation of recovery. Every effort you make toward understanding your mind, reaching out for help, or supporting others brings you closer to healing. You are not alone, and things can get better.
One of the most important truths about mental health is that you can get better. Recovery is not only possible, it is expected. For many people, this simple message can be the spark that begins their healing.
The way we deliver mental health care is evolving. Health systems and treatment centers around the world are rethinking how to reach more people effectively and efficiently. The goal is to provide just enough care to help people recover without overwhelming the system or the individual.
For example, researchers are looking at how many sessions of a particular psychotherapy are truly needed to make a difference. In many cases, combining traditional therapy with online programs, often called e-therapy, can shorten treatment time and make it more accessible. These digital tools allow people to work on their mental health between sessions, building new habits and insights at their own pace.
This new hybrid approach, which combines online work with direct sessions with a therapist, has been shown to be just as effective as traditional therapy for mild to moderate depression and anxiety. It also helps create more capacity so that more people can receive the support they need.
If you are starting treatment, remember three important points:
-
You can get better. The majority of people who seek treatment recover and return to a healthier, more balanced life.
-
Evidence-based care works. Ask your therapist what kind of treatment they are using. Therapy is most effective when it follows proven models such as cognitive behavioral therapy or other structured approaches that are supported by research.
-
Be open to new methods. Combining in-person and online support can increase flexibility and give you more tools to manage your mental health.
Understanding the Role of Hope
Feeling hopeless is often part of depression itself. The illness can distort how you see the world, convincing you that things will never improve. If you are struggling with this feeling, know that it is not a reflection of who you are but a symptom of the condition. Your mind may tell you that recovery is impossible, but the evidence says otherwise.
Mental health professionals understand this and are trained to support the part of you that still believes in getting better, even when your symptoms try to drown out that belief. The numbers are on your side. With the right treatment, many people begin to feel improvement in a matter of weeks.
What Is Mental Health First Aid?
Just as physical first aid teaches people how to help someone who is injured, Mental Health First Aid teaches people how to help someone who may be struggling emotionally or psychologically. The concept began in Australia more than two decades ago and has since spread around the world.
The goal of Mental Health First Aid is to train everyday people to recognize the signs of mental distress, respond with empathy, and connect someone to appropriate help. You do not need to be a professional to make a difference. What matters most is your ability to listen, communicate, and provide support without judgment.
Unlike physical first aid, there are no bandages or tools involved. The most important tool is communication. It is about learning how to approach someone who may be in crisis, or simply struggling quietly. Sometimes a single conversation can interrupt a downward spiral and give someone the courage to seek help.
Building a More Caring Community
When we invest in mental health, through education, open conversation, and effective services, we strengthen our communities. Every person who learns how to listen and respond with compassion becomes part of the solution.
Whether you are a healthcare worker, a teacher, a parent, or a friend, you have the power to make a difference. Learn how to recognize the signs of mental health struggles. Learn how to talk about them. And most importantly, remind others, and yourself, that recovery is possible.
Mental illness can feel dark and isolating, but there is always light ahead. With understanding, treatment, and hope, we can help one another find our way back to wellness.
How to Support Someone in Crisis: From Panic Attacks to Suicide Awareness
When someone you care about is struggling, it can be hard to know what to do or say. Many of us worry about saying the wrong thing or making the situation worse. Mental Health First Aid helps us move past that fear by giving us simple, practical tools to respond with confidence and compassion.
This training is not about becoming a counselor or a mental health professional. It is about learning how to recognize when someone might be in distress and how to respond in a supportive way. Just as traditional first aid teaches you to respond to physical injuries, Mental Health First Aid teaches you how to help someone who may be experiencing a mental health problem or crisis.
Supporting Someone Having a Panic Attack
If someone tells you they think they are having a panic attack, it can be frightening for both of you. The first thing to remember is to stay calm.
If you are unsure whether it is a panic attack or a heart attack, always call 911. Some people who are actually experiencing heart problems may assume it is just anxiety, so it is safer to let professionals assess the situation.
While waiting for help, or if you know it is a panic attack, gently guide the person to a quiet and safe space away from crowds or noise. People often feel trapped or embarrassed when panic symptoms begin, so privacy and reassurance go a long way.
Encourage slow, steady breathing. You can say something simple such as, “Let’s breathe together. Take a deep breath in, and let it out slowly.” Repeat this with them. Deep breathing can slow the heart rate and help the person regain a sense of control.
Avoid judgment or telling them to “calm down.” Instead, offer reassurance: “You are safe right now. This will pass, and I’m here with you.” Most panic attacks peak within minutes and begin to subside soon after.
Recognizing the Signs of Suicide Risk
Talking about suicide can feel uncomfortable, but it is one of the most important conversations you can have. People who are thinking about ending their life often give signs, but those signs can be easy to miss if you are not looking for them.
Training programs such as SafeTALK and ASIST (Applied Suicide Intervention Skills Training) are designed to help anyone recognize warning signs and learn how to respond. These courses teach people how to have open, nonjudgmental conversations and how to connect someone to professional help.
When you are concerned about someone, pay attention to four main areas:
-
Actions: Are they giving away belongings, withdrawing from friends and family, or talking about feeling like a burden?
-
Words: Are they mentioning hopelessness, saying others would be better off without them, or expressing that they want to die?
-
Feelings: Do they seem trapped, empty, or emotionally detached from life?
-
Situations: Have they recently experienced a major loss, trauma, or other serious stressor?
If you notice one or more of these warning signs, do not ignore them. Ask directly, “Are you thinking about suicide?” Research shows that asking the question does not cause harm. In fact, it can save a life by giving the person permission to speak honestly.
Stay with them if they are in immediate danger and reach out for professional help right away. If it is not an emergency, encourage them to speak with a doctor, counselor, or mental health crisis line.
You Can Make a Difference
You do not need to be an expert to help someone in crisis. What matters most is showing care, staying calm, and taking action when you notice the signs.
Mental health struggles are often invisible, but your willingness to listen and respond can bring someone comfort and hope. Every conversation counts, and every act of support helps build a community where people know they are not alone.
By learning the basics of Mental Health First Aid, you can be that calm, steady presence for someone when they need it most.
Recognizing and Responding to Suicide Risk
Sometimes the signs that someone is thinking about suicide are right in front of us, but we do not realize what they mean. Other times we sense something is wrong without being able to explain why. Learning to recognize these warning signs and knowing how to respond can save lives.
There are four main areas we can focus on.
The first is what we see. Pay attention to a person’s actions. If someone begins giving away personal possessions or withdrawing from family and friends, these changes may be signs of distress.
The second is what we hear. Listen closely to the things people say. You might hear comments such as, “I feel so alone,” or “I’m a burden on everyone.” Sometimes people will be direct and say, “I’m thinking of ending my life.” These are important statements to take seriously and never ignore.
The third area is what we learn. Major life events such as trauma, loss, or ongoing grief can increase a person’s risk. When someone has faced multiple painful experiences, it is worth paying closer attention and offering extra support.
Finally, there is what we sense. You might have a gut feeling that something is not right. That inner signal, what some call a spidey sense or intuition, is often worth trusting.
If you notice any of these signs, the best thing you can do is ask directly, “Are you having thoughts of suicide?” Many people worry that asking this question might put the idea in someone’s head, but that is a myth. Talking about suicide does not cause suicide. In fact, it gives the person a chance to open up about something they may have been too afraid or ashamed to say out loud.
People who think about suicide often feel isolated and hopeless. They may believe no one will understand. By asking and listening without judgment, you show that they are not alone. Research tells us that the more people who offer support family, friends, coworkers, and professionals, the greater the chance the person will survive and recover.
Sometimes people will deny having suicidal thoughts even when you suspect otherwise. That can happen for many reasons, including fear, embarrassment, or surprise that someone noticed. If you still feel uneasy, it is okay to ask again later or gently remind them of what they shared before. For example, you might say, “I know you said no, but earlier you mentioned that life doesn’t feel worth living and you’ve been giving away special belongings. That makes me concerned, and I just want to check in again.” Even if they continue to deny it, you have opened the door for future conversation.
If you want to learn more about how to recognize and respond to suicide risk, I encourage you to visit mentalhealthcapacity.org. You can also reach out by email at mentalhealthcapacity@gmail.com if you want guidance or help organizing a course.