Understanding Major Depression: The Science, Symptoms, and Steps Toward Healing
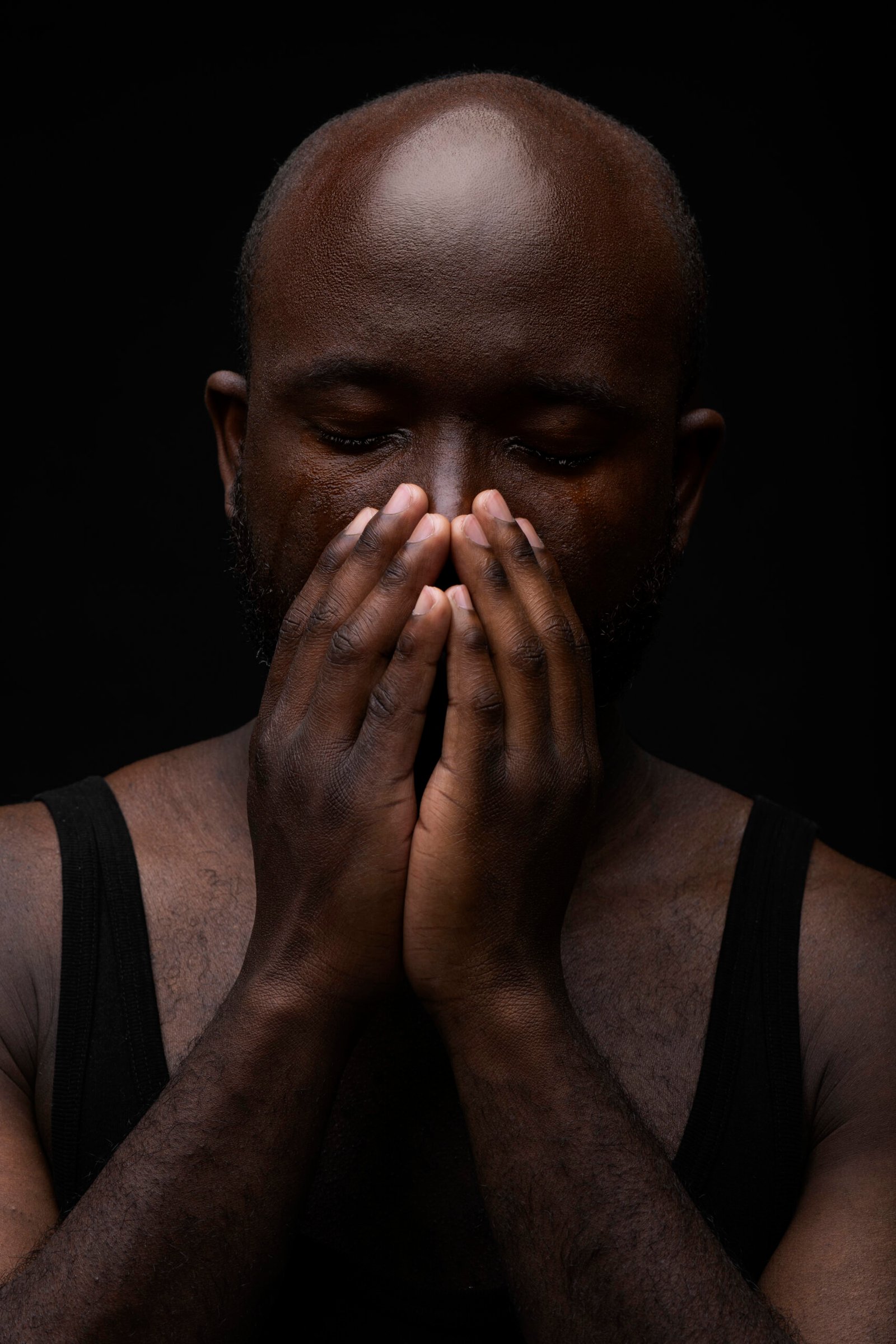
Depression is one of the most common and misunderstood mental health conditions in the world, quietly affecting millions of people across every age group and background. It is more than a fleeting sadness or a rough week; depression can deeply alter how a person feels, thinks, and functions. For many, it brings a persistent sense of emptiness, fatigue, or hopelessness that seems to have no clear cause. Yet behind this emotional fog lies a complex relationship between the brain, body, and environment , one that, when understood, can lead to real and lasting healing.
What Major Depression Really Is
Major depression, also known as clinical or unipolar depression, is characterized by ongoing sadness, loss of interest in daily life, and an inability to experience pleasure, a condition known as anhedonia. These emotional changes are often accompanied by feelings of guilt, self-blame, or worthlessness that don’t match reality. People may begin to believe that they are failing or undeserving of happiness, even when this is far from the truth. This distorted inner dialogue is one of the hardest parts of depression, but it is also one of the most treatable aspects when addressed through therapy, support, and lifestyle changes.
How Depression Affects Both Mind and Body
Depression doesn’t stop at emotions; it affects the body in noticeable ways. Many people experience disrupted sleep , either waking up too early or sleeping much longer than usual but still feeling tired. Appetite can change as well, with some people eating far less and others turning to food for comfort. These physical shifts, often called vegetative symptoms, reflect the deep connection between mental and physical health. When the body’s stress systems go off balance, energy levels drop, motivation fades, and even simple daily tasks can feel overwhelming.
The stress hormone cortisol, which should rise in the morning and fall at night, often stays elevated into the evening in people with depression. This irregular rhythm can make it harder to rest, focus, or maintain stable energy throughout the day. Over time, this imbalance contributes to emotional exhaustion and physical fatigue, reinforcing the cycle of low mood.
The Brain Chemistry Behind Depression
Inside the brain, depression is linked to changes in three key neurotransmitters , serotonin, dopamine, and norepinephrine. These chemical messengers regulate mood, motivation, and energy. Serotonin helps create emotional stability and calm, dopamine fuels drive and pleasure, and norepinephrine keeps us alert and focused. When these systems become disrupted, the brain struggles to maintain balance, leading to sadness, low energy, and disinterest in life.
Antidepressant medications are designed to help restore this balance by enhancing the activity of these neurotransmitters. However, because everyone’s brain chemistry is unique, treatments that work for one person may not work for another. That’s why recovery often involves a combination of medical care, therapy, and lifestyle adjustments that support brain and body harmony.
The Impact of Stress, Hormones, and Inflammation
Chronic stress is one of the most powerful triggers for depression. When stress hormones like cortisol remain high for long periods, they interfere with serotonin and dopamine signaling. This ongoing tension can drain both emotional and physical energy, making it harder to stay motivated or optimistic. Hormonal changes also play a role , especially after childbirth, during the menstrual cycle, or at menopause — as shifts in estrogen, progesterone, and thyroid activity can influence mood.
Modern research has also uncovered a strong connection between inflammation and depression. When the immune system stays active for too long, it releases inflammatory molecules that can interfere with brain chemistry and mood regulation. Inflammation may even block the production of serotonin, leading to increased sadness and fatigue. Reducing inflammation through diet, exercise, and sleep is therefore a powerful step toward emotional recovery.
Practical Tools for Everyday Healing
Healing from depression rarely happens overnight, but consistent daily actions can make a remarkable difference. Movement, for example, is one of the most powerful natural antidepressants. Physical activity increases levels of serotonin, dopamine, and norepinephrine , the same chemicals that medications target. Even a brisk 20-minute walk or light stretching can lift mood and improve energy.
Sleep plays a major role as well. Keeping a regular sleep schedule and getting sunlight within an hour of waking can reset the body’s internal clock and stabilize hormones. Nutrition supports this process too. Foods rich in omega-3 fatty acids, particularly EPA and DHA found in fish oil, help protect brain cells and lower inflammation. B vitamins, magnesium, and protein also support neurotransmitter production, helping the brain recover more efficiently.
Social connection and purpose are equally vital. Sharing experiences with others, volunteering, or pursuing a personal goal can reignite motivation and strengthen feelings of belonging. Human connection releases oxytocin and dopamine ,two powerful mood-boosting chemicals that help rebuild emotional balance.
Emerging Therapies and Hopeful Discoveries
For those who do not respond to traditional treatments, new therapies are offering renewed hope. Medical research is exploring the use of ketamine and psilocybin (a naturally occurring compound found in certain mushrooms) in controlled clinical settings to help people reframe self-critical thought patterns and strengthen neural connections associated with positive mood. Creatine, a natural supplement known for improving physical energy, may also enhance mood and the effectiveness of antidepressants. Additionally, ketogenic diets, which encourage the body to use fats rather than sugars for energy, have shown promise in supporting brain function and stabilizing mood in some individuals.
While these approaches are still being studied, they remind us that depression is treatable and that science continues to uncover new ways to restore mental well-being.
Moving Forward With Compassion and Strength
Depression is not a personal failure, it is a condition that arises from the complex interaction of biology, stress, and life experience. Healing requires patience and compassion — not only from others but from oneself. The same brain that once reinforced negative thoughts can, with time and care, learn new patterns of resilience, calm, and hope.
Combining therapy, lifestyle changes, medical care, and community support can create a strong foundation for recovery. Even small steps — taking a walk, reaching out to a friend, practicing deep breathing , signal to the brain that change is possible. Every positive choice strengthens the pathways toward healing and growth.
If you or someone you care about is struggling with depression, remember that help is always available. With the right tools and support, it is entirely possible to rediscover balance, connection, and joy. The human mind is incredibly adaptable, and healing is not only possible — it is within reach for everyone willing to take the first step.
Frequently Asked Questions About Major Depression
1. What is major depression?
Major depression, also known as clinical depression, is a serious mental health condition that causes persistent feelings of sadness, emptiness, or hopelessness. It affects how a person thinks, feels, and behaves, often interfering with daily activities, relationships, and overall quality of life. It is not simply feeling sad or having a bad day — it is a long-term condition that requires understanding and care.
2. What are the main symptoms of depression?
Symptoms can include deep sadness, loss of interest in activities once enjoyed, fatigue, changes in appetite or sleep patterns, difficulty concentrating, and feelings of guilt or worthlessness. Some people experience physical symptoms such as body aches, headaches, or digestive issues. In severe cases, depression can lead to thoughts of self-harm or suicide, which should always be treated as a medical emergency.
3. What causes depression?
Depression is caused by a combination of biological, psychological, and environmental factors. Imbalances in brain chemicals such as serotonin, dopamine, and norepinephrine can contribute to low mood. Stress, trauma, chronic illness, hormonal changes, and genetics can also play important roles. Often, it is not one single cause but several interacting influences that lead to depression.
4. How does stress contribute to depression?
When the body experiences long-term stress, it releases high levels of cortisol, a hormone that helps manage danger and alertness. Over time, elevated cortisol disrupts the brain’s normal balance and reduces serotonin and dopamine activity, leading to feelings of exhaustion, irritability, and sadness. Managing stress through rest, mindfulness, and relaxation can help reduce this risk.
5. Can depression affect physical health?
Yes, depression and physical health are closely connected. Depression can weaken the immune system, increase inflammation, and disturb sleep and appetite patterns. It can also worsen chronic conditions such as heart disease or diabetes. This is why treating depression often improves overall physical well-being as well as mental health.
6. What are the best treatments for depression?
There is no one-size-fits-all solution, but treatment often includes therapy, medication, lifestyle changes, or a combination of these. Cognitive Behavioral Therapy (CBT), interpersonal therapy, and mindfulness-based therapy are proven to help people recognize and change negative thought patterns. Antidepressant medications may help balance brain chemistry, while exercise, sleep, and proper nutrition support long-term recovery.
7. Are there natural ways to manage depression?
Yes. Regular physical activity, exposure to morning sunlight, a balanced diet rich in omega-3 fatty acids, and consistent sleep routines can all improve mood naturally. Social connection, gratitude practices, and mindfulness can reduce stress and boost emotional resilience. These methods work best when combined with professional care.
8. What new treatments are available?
Emerging therapies like ketamine infusions, psilocybin-assisted therapy, and creatine supplementation are showing promise for people who don’t respond to standard treatments. These therapies are offered in controlled clinical settings and can help reshape brain circuits that influence mood. Ongoing research continues to uncover safer and more effective approaches.
9. Can genetics make someone more prone to depression?
Yes, family history can increase the likelihood of developing depression. If a close relative has experienced depression, the risk is higher, but genes are not destiny. Environmental factors, lifestyle, and stress management play equally important roles in preventing and managing depression.
10. How can I support someone who is depressed?
The most important thing you can do is to listen without judgment. Offer empathy, encourage professional help, and check in regularly. Simple acts of kindness and presence can make a huge difference. Avoid giving unsolicited advice or minimizing their pain — instead, remind them that they are not alone and that help is available.
11. Can depression be cured?
Many people recover fully from depression, while others learn to manage it successfully over time. With treatment, lifestyle adjustments, and support, symptoms can significantly improve or disappear. Healing is a process, and with the right tools, balance and joy can absolutely return.
12. When should I seek professional help?
If feelings of sadness, hopelessness, or lack of motivation persist for more than two weeks, or if you notice thoughts of self-harm, it’s time to reach out for professional help. A licensed therapist, counselor, or medical doctor can assess your situation and guide you toward the most effective treatment plan. Seeking help is not a sign of weakness — it’s a powerful step toward healing.